The discovery of the IL-23 pathway and elucidation of its role in autoimmunity has led to a paradigm shift within the field of immunology. Decades ago, T cells were divided into CD4+ helper and CD8+ killer T cell categories, with CD4 T cells later being further divided into Th1 and Th2 categories.1 Since its discovery in the early-1990s, the most important function of IL-12 has been recognized to be its regulation of the differentiation of naïve T cells into Th1 cells.2-5 The ability of IL-12 to promote the development of gamma interferon (IFN-γ) producing Th1 cells led to the widely-held belief that its dysregulation underlies several autoimmune diseases. This paradigm of IL-12 as a regulator of inflammation and autoimmunity was supported by preclinical studies in mice deficient in the cytokine (p40-/- mice), which were resistant to experimentally-induced autoimmunity.6-10 However, other data were difficult to explain using this paradigm. For example, while Th1 cells were thought to be responsible for multiple sclerosis (MS), treating mice in the mouse model of MS (experimental autoimmune encephalitis [EAE]) with the Th1 cytokine IFN-γ alleviated disease, while blocking it enhanced disease severity.11,12
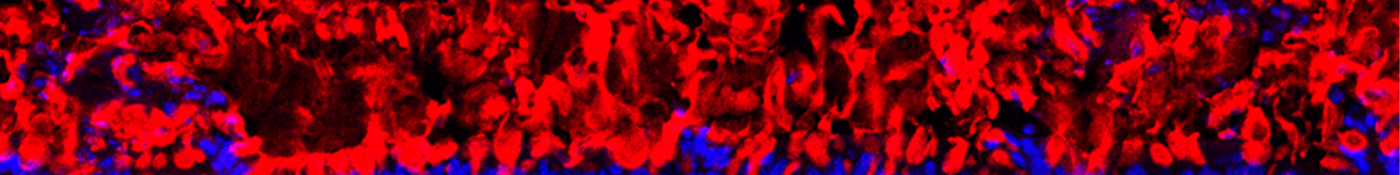
These inexplicable findings were explained years later when it was discovered that an IL-12-related cytokine, IL-23, shares a common subunit with IL-12, the p40 subunit. However, in IL-23 this p40 subunit pairs with a distinct/unique p19 subunit.13 Furthermore, rather than driving differentiation of a T cell subset, as IL-12 does, IL-23 was shown to mature a population of T cells already differentiated by other cytokines (TGFβ and IL-6), allowing them to acquire a pathogenic, inflammatory phenotype.6,14-19 IL-23 was found to expand and maintain this cell population with a unique inflammatory gene signature that includes several IL-17 genes, leading to the nomenclature for this novel subset of T helper cells as Th17 cells.6,20-22 Suddenly, it became clear that the roles previously attributed to IL-12 in some autoimmune diseases were instead regulated by IL-23. In support of this idea was the finding that mice deficient in the IL-12/IL-23 p40 subunit are resistant to a variety of autoimmune conditions (including EAE), while mice deficient in the other IL-12 subunit, IL-12 p35, were either unprotected or demonstrated exacerbated disease.6-10 Similarly, it has been reported in preclinical studies that IL-23 in murine skin is responsible for the excessive growth and abnormal differentiation of keratinocytes underlying psoriasis, while IL-12 does not promote this pathology.23-30
Genetic studies have linked IL-23R polymorphisms with susceptibility to psoriasis, psoriatic arthritis, ankylosing spondylitis, multiple sclerosis, and Crohn’s Disease, demonstrating a role for this pathway in regulating many forms of autoimmunity.31-35 Additionally, elucidation of this pathway has also dispelled some of our previous false notions, such as the notion that inflammation is universally beneficial in fighting cancer, which was disproven by preclinical models demonstrating that IL-23 promotes tumorigenesis.36-40
This paradigm shift in which it was realized that IL-23 is also a regulator in autoimmune disease spurred on research aimed at interrogating the regulation and function of the IL-23 pathway and its players, including Th17 cells.41 Initially, the role of IL-23 and IL-17 in promoting autoimmune disease was thought to be vastly overlapping, however this too has proven to be an oversimplification of a more complex system of immune regulation. For example, mice without IL-23 were found to be resistant to EAE, while those deficient in IL-17 had attenuated disease.6,42,43 Further adding to the complexity of the system, we now know that Th17 cells themselves can have divergent functions. In fact, Th17 activity is determined by the balance of cells activated by TGFβ and IL-6, which curtail immunopathogenic responses, versus those activated by IL-23, which promote chronic inflammation and autoimmunity. IL-23 acts late in the development of Th17 cells. Thus, Th17 cells initially induced with TGFβ and IL-6 require exposure to IL-23 in order to develop full pathogenic potential.14,44-48 As such, Th17 cells can exert different effects depending on the tissue micro environment.
Additional distinction in the roles of IL-23 and IL-17 can likely be explained by the discovery that IL-23 controls important effector functions beyond maintaining and conferring pathogenicity on Th17 cells. Consistent with the rapidity of tissue responses to IL-23, innate cells have been discovered which respond directly and immediately to this cytokine. Indeed, many such cells can respond to IL-23, including subsets of γδ T cells, natural killer T (NKT) cells, and innate lymphoid cells (ILCs). These are predominantly located in non-lymphoid tissue and respond to IL-23-stimulation by producing proinflammatory cytokines (IL-17, IL-22, and IFN-γ), thereby inducing local tissue inflammation.20, 23, 49, 50 We are now starting to appreciate that downstream effects of IL-23R engagement are dependent not only on the cell population expressing the IL-23 receptor, but also the environment (organ) within which those cells reside, ultimately allowing for divergent roles and effector functions depending on the disease.
Discovery of the IL-23 pathway is just the beginning. There remains a tremendous amount of work needed to elucidate the role of this pathway in various autoimmune diseases and to understand its interplay with other regulatory players. Janssen is committed to exploring this pathway and further elucidating its role in autoimmunity. In fact, we are exploring the role of IL-23 in diseases in rheumatology, gastroenterology and immunodermatology. If you have a desire to redefine treatments for immune diseases, consider joining Janssen Immunology, where we’re working to deliver transformational and accessible therapies and regimens to patients with autoimmune disease.