Why Evaluating Healthcare Quality of Life is Critical in the Treatment of Crohn’s Disease
Crohn’s disease (CD) has a tremendous impact on the health and well-being of people living with the condition, causing physical burdens that can include abdominal pain and tenderness, frequent diarrhea, rectal bleeding, weight loss and fever.[1] The disease may also have manifestations beyond intestinal symptoms and gut dysfunction, such as anxiety and depression, which can be caused by, or contribute to, a patient’s symptom experience.[2][3]
These unmet needs inspire Janssen and I in our commitment to conduct new research into the impact of treatment on patients, like the findings we are presenting at this year’s annual United European Gastroenterology (UEG) Week congress.
The physical and psychological burden of Crohn’s disease
Along with ulcerative colitis (UC), CD is one of the main forms of inflammatory bowel disease (IBD)[4] for which there is currently no known cause or cure.[5][6] CD is often diagnosed in adolescents or adults between the ages of 20 and 30.[4][6][2] Given that many people are diagnosed at a relatively young age, they can face a lifetime of challenges relating directly to the symptoms and complications of their disease as well as the condition’s impact on their psychological well-being, and related challenges navigating life events.[2]
Despite strides in treatment, a considerable number of people with IBD do not respond to available therapies or can lose response over time.[6][7][8] A recent study showed that CD flare-ups can negatively impact daily life, work productivity, emotional well-being, and result in high levels of healthcare resource usage.[9] It is not surprising that the physical, economic, and psychosocial burden of CD leads to impaired or poor health-related quality of life (HRQoL).[10]
The importance of screening for HRQoL
The therapeutic goals for IBD are to control disease flares, alleviate symptoms and, ultimately, improve patients’ HRQoL.[10] A large body of evidence has consistently shown that patients with active IBD in relapse have significantly decreased HRQoL.[10] While diminishing disease activity or inducing remission can help improve HRQoL, studies have also shown that a large number of IBD patients have reported low HRQoL despite being in remission.[10] Understanding the factors that impact HRQoL may help facilitate both the development of interventions that can improve it and IBD management overall.[11]
In clinical research and practice, evaluation of HRQoL has been increasingly used to provide insight into patients’ perceptions of their health and treatment effectiveness, and to compare effects of different treatment strategies.[10]
Measuring treatment impact on HRQoL using PROMIS-29
One tool that is used to assess HRQoL is the National Institutes of Health PROMIS (Patient-Reported Outcomes Measurement Information System), a set of person-centered measures that evaluates and monitors physical, mental and social health in adults and children.[12] PROMIS was established to develop and validate patient-reported health and well-being outcomes for clinical research and practice.[13][14] These self-assessments provide rapid, efficient and valid identification of patients who may then be evaluated for further psychosocial interventions.[3]
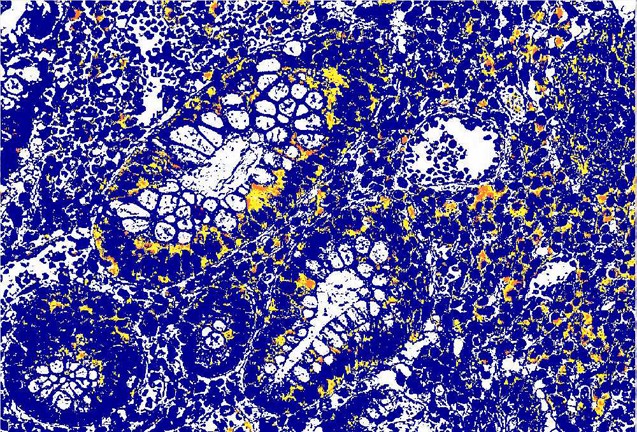
Janssen is committed to researching the impact of treatment on patients’ HRQoL. This year at UEG Week, our researchers presented data from a study assessing HRQoL among patients with moderately to severely active CD who had inadequate response or intolerance to prior therapies (both conventional therapies and/or biologics).[15] At baseline, the different treatment groups in this study had similarly impaired HRQoL.
We evaluated HRQoL using PROMIS-29 – a tool to assess four items in each of seven domains (depression, anxiety, physical function, pain interference, fatigue, sleep disturbance, and social participation) – along with a pain intensity 0-10 numeric rating scale.[14][16] By the end of this study, patients treated with the study drug had greater improvement in all seven domain scores.
These new study outcomes are encouraging, as it is evident that aiming for clinical or biochemical remission alone is not enough considering psychological health is also an important driver of disease activity.[15] At Janssen, we are committed to addressing the complex burdens people with IBD and other immune-mediated diseases experience throughout their patient journey, with the aim of improving their everyday lives. This data being presented at UEG Week is just one example of how we are working to do so.
#UEGWeek #CrohnsDisease #IBD #Gastroenterology #Immunology #MyCompany
Since we’re on LinkedIn, I invite you to explore our career opportunities at Janssen Immunology: https://bit.ly/3CXFabC.
To learn more about our presence at this year’s UEG Week, please visit: https://bit.ly/3BXzoGh.
References
1. Crohn’s & Colitis Foundation. Signs and Symptoms of Crohn’s Disease. Available at: https://www.crohnscolitisfoundation.org/what-is-crohns-disease/symptoms. Accessed August 2022.
2. IsHak, W.W., et al. Patient-Reported Outcomes of Quality of Life, Functioning, and GI/Psychiatric Symptom Severity in Patients with Inflammatory Bowel Disease (IBD). Inflamm Bowel Dis. 2017 May;23(5):798-803. https://doi.org/10.1097/MIB.0000000000001060
3. Pan, D., et al. Validation and Utility of Patient-Reported Outcomes Measurement Information System (PROMIS) in an Ambulatory Adult Inflammatory Bowel Disease (IBD) Care Setting: 1897. Am. J. Gastroenterol. 2015 Oct;110:S806. https://doi.org/10.14309/00000434-201510001-01897
4. Crohn’s & Colitis Foundation. Overview of Crohn’s Disease. Available at: https://www.crohnscolitisfoundation.org/what-is-crohns-disease/overview. Accessed August 2022.
5. Crohn’s & Colitis Foundation. What is Crohn’s disease? Available at: https://www.crohnscolitisfoundation.org/what-is-crohns-disease/causes. Accessed August 2022
6. Mayo Clinic. Crohn’s disease. Available at: https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304. Accessed August 2022.
7. Fine, S., Papamichael, K., Cheifetz, A.S. Etiology and Management of Lack or Loss of Response to Anti-Tumor Necrosis Factor Therapy in Patients With Inflammatory Bowel Disease. Gastroenterol Hepatol (N Y). 2019 Dec;15(12):656-665. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6935028/
8. Mayo Clinic. Ulcerative Colitis. Available at: https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-causes/syc-20353326. Accessed April 2022.
9. Sanon, M. et al. Impact of Disease Flares of Resource Use, Health-related Quality of Life and Productivity in Patients with Crohn’s Disease in the United States: An Analysis of National Health and Wellness Survey Data. Presented at DDW 2022, May 21-24.
10. Fu, H., et al. Associations between disease activity, social support and health-related quality of life in patients with inflammatory bowel diseases: the mediating role of psychological symptoms. BMC Gastroenterol 20, 11 (2020). https://doi.org/10.1186/s12876-020-1166-y
11. Moradkhani, A. et al. Health-related quality of life in inflammatory bowel disease: Psychosocial, clinical, socioeconomic, and demographic predictors. J Crohns Colitis. 2013 Jul;7(6):467-73. https://doi.org/10.1016/j.crohns.2012.07.012
12. The NIH Patient-Reported Outcomes Measurement Information System. Available at: http://www.healthmeasures.net/explore-measurement-systems/promis. Accessed August 2022.
13. National Institute on Aging. Patient-Reported Outcomes Measurement Information System (PROMIS). Available at: https://www.nia.nih.gov/research/resource/patient-reported-outcomes-measurement-information-system-promis. Accessed August 2022.
14. Kwakkenbos, L., Thombs, B.D., Khanna, D., Carrier, M.E., Baron, M., Furst, D.E., Gottesman, K., van den Hoogen, F., Malcarne, V.L., Mayes, M.D., Mouthon, L., Nielson, W.R., Poiraudeau, S., Riggs, R., Sauvé, M., Wigley, F., Hudson, M., Bartlett, S.J.; SPIN Investigators. Performance of the Patient-Reported Outcomes Measurement Information System-29 in scleroderma: a Scleroderma Patient-centered Intervention Network Cohort Study. Rheumatology (Oxford). 2017 Aug 1;56(8):1302-1311. https://doi.org/10.1093/rheumatology/kex055
15. Fairbrass, K.M., et al. Relative Contribution of Disease Activity and Psychological Health to Prognosis of Inflammatory Bowel Disease During 6.5 Years of Longitudinal Follow-Up. Gastroenterology. 2022 Jul;163(1):190-203.e5. https://doi.org/10.1053/j.gastro.2022.03.014
16. D’Haens G., et al. Presented at UEG Week, Oct. 8-11, 2022.
Hospital Israelita Albert Einstein, MD, MACG
1y👋👋👋