Precision medicine and the need for greater adoption
As we settle into a new year, we look ahead in hope for new innovation and treatments with the potential to revolutionise cancer care. Before the 2023 American Society of Clinical Oncology Genitourinary Cancers (ASCO GU) Symposium kicks off later this week, I find myself thinking back to my days as a medical student where precision medicine was abstract and its full potential hadn’t yet been appreciated. ASCO GU serves as another reminder of the progress we’ve made, the chapter of constant change we’re in, and how much more we have to do. The more we discover, the more we realise no two cancers are the same. If we want to intercept, to eliminate or redefine the course of cancer, we urgently need to be able to tailor care to a patient’s individual characteristics.[1]
What is the potential of precision medicine?
Precision medicine is a healthcare approach that uses diagnostic tests, imaging and health information to inform personalised treatment decisions, and ultimately aims to improve health outcomes.[2] Recognising each patient is unique; it enables us to move further from the “one size fits all” approach by using individual characteristics, called biomarkers, to screen, diagnose and monitor patients and so to ideally prevent or intercept, or at least to improve the management of cancer.[2]
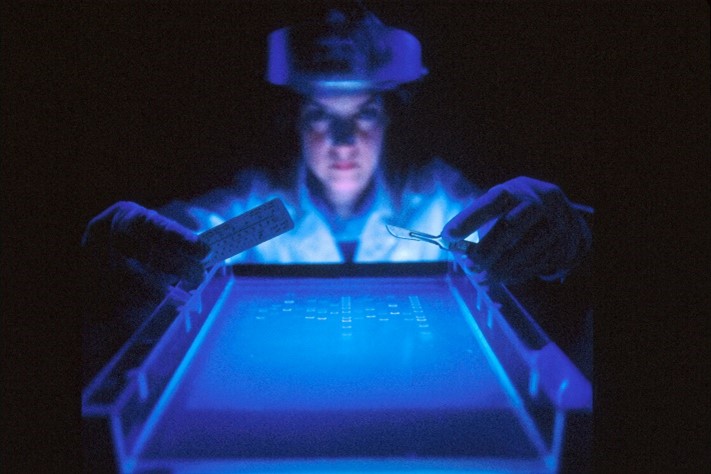
The use of diagnostic tools, such as next generation sequencing (NGS), allow us to detect genetic alterations, which drive tumour growth and identify drugs tailored to target these oncogenic pathways.[3] Advances in biomarker testing are contributing to the shift towards precision medicine within oncology.[1] Their use provides vital insights into how the disease might develop and how a patient might respond to certain treatment.[1]
So the potential of precision medicine is varied and profound.[2] Undoubtedly, precision medicine can provide better outcomes for patients, as well as reduce the risk of adverse effects.[2] But, not only that, precision medicine approaches ensure healthcare systems are more sustainable by identifying which interventions are likely to be of most benefit to a patient or group of patients and avoid overtreatment;[4] it can help patients, physicians, payers and healthcare providers identify disease and at-risk populations earlier; it can provide all stakeholders the confidence that the chosen treatment has the best chance of working; and it can improve clinical trial recruitment and efficiency, and therefore effectiveness.2,[5]
What is holding precision medicine back in Europe?
Biomarkers and biomarker testing are essential components of precision medicine and allow for accurate treatment decisions.[1] Considerable progress has been made in the understanding of biomarkers and therapies linked to biomarkers in oncology, with around 55% of all oncology clinical trials in 2018 involving the use of biomarkers, compared with around 15% in 2000.[6] However, the prevalence, uptake and access to biomarker testing within oncology is inadequate and inconsistent across countries in Europe.[1],[7] Variables that affect the access of biomarker testing and precision medicine across Europe include (but are not limited to) public reimbursement and funding processes, presence of appropriate laboratory infrastructure and capabilities,[8] stakeholder awareness and education,[1] and Health Technology Assessment (HTA) processes.[7]
Where do we go from here?
Across Europe, significant changes to precision medicine policy, environment, understanding and implementation need to be made in order to enable improvements in the provision of cancer care.[7] Improving public funding to support biomarker testing, as well as enhancing stakeholder awareness and education will drive and support the widespread use of precision medicine within oncology.[1] Precision medicine and biomarker testing are quickly rising to the forefront of oncology research, and there is need for the industry to adapt to this evolving standard of cancer care.[6]
If you are interested in learning more, I encourage you to listen to my colleague Laetitia Decroix Gullioux’s interview with Oncology Central, in an episode entitled ‘why personalised medicine is vital to managing lung cancer’, from the societal impact to prevention and interception. Listen to the podcast here.
[1] Unlocking the potential of precision medicine in Europe. Improving cancer care through broader access to quality biomarker testing. Policy recommendations. IQN Path, European Cancer Patient Coalition and EFPIA. Feb 2021. Available at: https://ecpc.org/wp-content/uploads/2021/03/unlocking-the-potential-of-precision-medicine-in-europe-23022021.pdf. Last accessed: February 2023.
[2] Definition adapted from EFPIA Precision Medicine Working Group https://www.efpia.eu/about-medicines/development-of-medicines/precision-medicine/#:~:text=%E2%80%9CPrecision%20medicine%20is%20a%20healthcare,resulting%20in%20improved%20health%20outcomes%E2%80%9D Last accessed February 2023.
[3] What is a Biomarker? NursingCenter Blog. 2019. Available at: https://www.nursingcenter.com/ncblog/november-2019/biomarker
[4] Vicente et al. How personalised medicine will transform healthcare by 2030: the ICPerMed vision. J Transl Med 18, 180 (2020).
[5] Precision Medicine: Its Impact on Clinical Trials and Orphan Drugs. Anju Software. 2019. Available at: https://www.anjusoftware.com/about/all-news/insights/precision-medicine. Last accessed: February 2023.
[6] The Evolution of Biomarker use in Clinical trials for Cancer Treatments. Key Findings and Implications. Vadas, Bilodeau, and Oza. PMC (Personalized Medicine Coalition) and L.E.K consulting. 2020. Available at: https://www.personalizedmedicinecoalition.org/Userfiles/PMC-xCorporate/file/The_Evolution_of_Biomarker_Use_in_Clinical_Trials_for_Cancer_Treatments.pdf. Last accessed February 2023.
[7] Gill, et al. ‘Access to Personalised Oncology in Europe’. 2020. London School of Economics. Available at: https://www.efpia.eu/media/580518/access-to-personalised-oncology-in-europe.pdf. Last accessed: February 2023.
[8] Normanno et al. Access and quality of biomarker testing for precision oncology in Europe. EJC. 2022; 176: 70-77



